NOT ALL CLINICS ARE CREATED EQUAL.
Don’t assume that a clinic claiming to specialize in hemorrhoid treatment is staffed with board certified colon rectal surgeons. Here at CRS, our experienced team of board certified colon rectal surgeons provides hemorrhoid patients with the best quality care for this common medical problem.
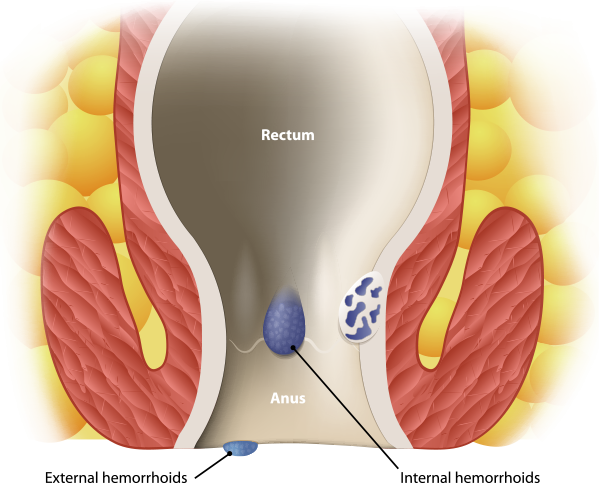
Because rectal bleeding is often the result of factors other than hemorrhoids, it is best to consult with a board certified specialist to determine the best treatment program for anal rectal problems.
Call us to schedule an appointment