CROHN’S / ULCERATIVE COLITIS
INFLAMMATORY BOWEL DISEASES
INFLAMMATORY BOWEL DISEASES
Crohn’s Disease and Ulcerative Colitis are the most common examples of conditions known as Inflammatory Bowel Disease, or “IBD” for short. There are actually many possible reasons for a patient to suffer intestinal inflammation, including infectious causes or blood supply issues. Both Crohn’s Disease and Ulcerative Colitis share the fact that they are both of common and, to date, of unknown cause (idiopathic).
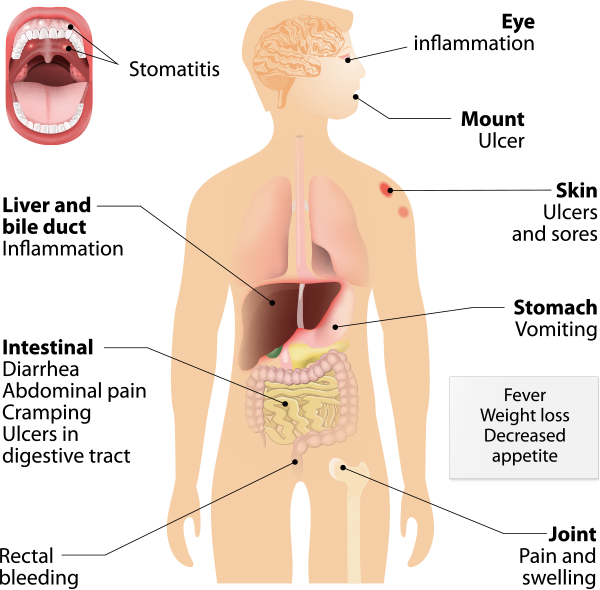
Crohn’s Disease affects men and women in almost equal numbers. About one fifth of the people diagnosed with Crohn’s Disease have a blood relative – most often a brother or sister – who have some form of IBD. Crohn’s Disease creates inflammation usually in the small intestine and colon, but can affect any part of the digestive tract. Crohn’s Disease is sometimes referred to as “ileitis or enteritis” because it commonly affects the end of the small intestine, the terminal ileum. Inflammation from Crohn’s Disease often causes diarrhea, abdominal pain and weight loss.
Like Crohn’s Disease, Ulcerative Colitis is a form of bowel inflammation, but it is limited to the lining of the large intestine causing ulceration. The most common symptom of Ulcerative Colitis is bloody diarrhea.
These inflammatory conditions should be distinguished from Irritable Bowel Syndrome (IBS) which is a functional bowel disorder where there is no evidence of bowel inflammation to correspond to a patients symptoms.
A diagnosis of inflammatory bowel disease is made based on patient symptoms, physical examination, and laboratory and diagnostic testing. Stool evaluations to rule out infectious causes of inflammation are important. Laboratory tests might document evidence of blood loss.
A critical step in the patient’s evaluation involves examination of the intestine with a fiberoptic instrument called a colonoscope. Under light sedation the entire large intestine can be inspected and biopsies can be performed for microscopic evaluation. Usually the most terminal portion of the small intestine can be visualized as well. Occasionally, colonoscopy might be supplemented by X-Ray testing or even “capsule endoscopy” which has caught the public’s imagination as the “camera pill.”
Crohn’s: Crohn’s Disease can affect any part of the gastrointestinal tract from the mouth to the anus. The symptoms are related to the location of the disease and the severity. The most common symptoms of Crohn’s Disease are abdominal pain – often in the lower right area – and diarrhea. Children with Crohn’s Disease may suffer delayed development and stunted growth.
Ulcerative Colitis: Ulcerative colitis only affects the colon and rectum. The symptoms are related to the extent of inflammation. As mentioned previously, the most common symptom of Ulcerative Colitis is bloody diarrhea. The inflammation begins in the end of the large intestine, the rectum, and then extends upstream (proximally) to involve greater or lesser amounts of the colon.
There are several theories about the causes of Crohn’s Disease and Ulcerative Colitis, the most popular of which is that the inflammation in the intestine is caused by the body’s immune system reacting to a virus or bacteria. This theory is buoyed by the fact that people with Crohn’s Disease and Ulcerative Colitis tend to have abnormalities of the immune system or autoimmune diseases. Like the classic example of the chicken or the egg, however, medical science still doesn’t know which came first. One thing we’re sure of, however, is that Crohn’s Disease is not caused by emotional stress – but for those afflicted, Crohn’s Disease is indeed very stressful.
The treatment of intestinal inflammation is both medical and surgical. Many patients improve with simple medicines that reduce inflammation. More serious cases have traditionally been treated with medications called steroids, which are effective in the short term but have long term side effects that are unacceptable. Over the last 10 years, medications first introduced to treat certain cancer patients have been found to be effective in reducing the amount of steroids required by sicker patients. However, these medicines are complicated to administer and their benefits are slow in onset. These drugs are called immunomodulators and include azathioprine, 6 mercaptopurine and methotrexate.
In 1997, a new class of medications became available called “biologics”. These medications target the molecules that are produced by inflammatory cells and injure normal tissues. Since 2001, CRS has been administering these medications to benefit our patients diagnosed with Crohn’s disease. In December 2005, the FDA approved these medicines for patients diagnosed with ulcerative colitis as well.
Fortunately, the advent of this new generation of medications has had a tremendous impact on our patients diagnosed with bowel inflammation. Our surgical skills are nonetheless important in the management of patients who fail to respond to medications, or who suffer from damage done before these medicines were available. Any surgeon will tell you these can be very complicated situations and our specialization provides crucial skills and decision making to improve our patients’ outcomes. Some patients can be offered laparoscopic surgery. We offer restorative surgeries (ileoanal pouch anastomosis) for patients with more severe varieties of colitis.
What is most important to remember is that at CRS we have broad experience in all aspects of the diagnosis and treatment of inflammatory bowel disease including both medical and surgical treatment. Despite the fact that we are all board certified surgeons, we always strive to manage these conditions medically. We routinely perform IV therapy in the comfort of our office. We resort to more invasive measures only when it is absolutely necessary.